Learn about who we are, what we believe
and the people who lead us
Discover our unique scientific approach
for diseases with high unmet need
The first and only FDA-approved
treatment for Demodex blepharitis
Explore the possibilities of our robust pipeline
to address significant unmet patient needs
Find additional corporate
and stock information
Demodex blepharitis (DB) is a highly prevalent and underdiagnosed ocular disease that affects ~58% of eye care patients in the United States1-3,*
*Titan study: a retrospective chart review for DB by 7 investigators at 6 eye care clinics of the case records of patients (N=1032) who underwent a slit lamp examination regardless of chief complaint.1
Actual patient with DB.
Demodex mites are associated with more than two-thirds of blepharitis cases in the United States, which are characterized by eyelid margin inflammation, redness and irritation.1,2

Of the 45 million people who visit eye care clinics annually, ~58% have collarettes, the pathognomonic sign of DB1,3
In the United States, ~25 million eye care patients may have DB3
STUDY DESIGN: A retrospective chart review for DB by 7 investigators at 6 eye care clinics of the case records of patients (N=1032) who underwent a slit lamp examination, regardless of chief complaint.1
1.5 Million
patients with meibomian gland disease (MGD) diagnosed with DB1,4
1.5 Million
patients with blepharitis diagnosed with Demodex4
1.2 Million
patients treated for dry eye diagnosed with DB1,5,6
2.2 Million
patients with cataracts diagnosed with DB1,7
2.3 Million
patients with contact lens intolerance diagnosed with DB1,8
DB is caused by infestation of Demodex mites, the most common ectoparasite found on humans.2
DB is caused by infestation of Demodex mites, the most common ectoparasite found on humans.2
There are 2 species of Demodex — D. folliculorum and D. brevis — that live on the skin of the face and eyelids.2,9,10


Actual patient with DB.
Atlas study: A multicenter, observational, prospective study that included 311 patients with DB aged ≥18 years. DB was diagnosed based on the presence of ≥1 mite per lash (upper and lower eyelids combined), >10 collarettes on the upper lashes, and at least mild eyelid margin erythema of the upper eyelid in ≥1 eye. All patients were asked to complete a questionnaire about their symptoms, daily activities, quality of life, and management approaches, and descriptive statistics were used to analyze the responses.3
Impact of DB on daily life3,†
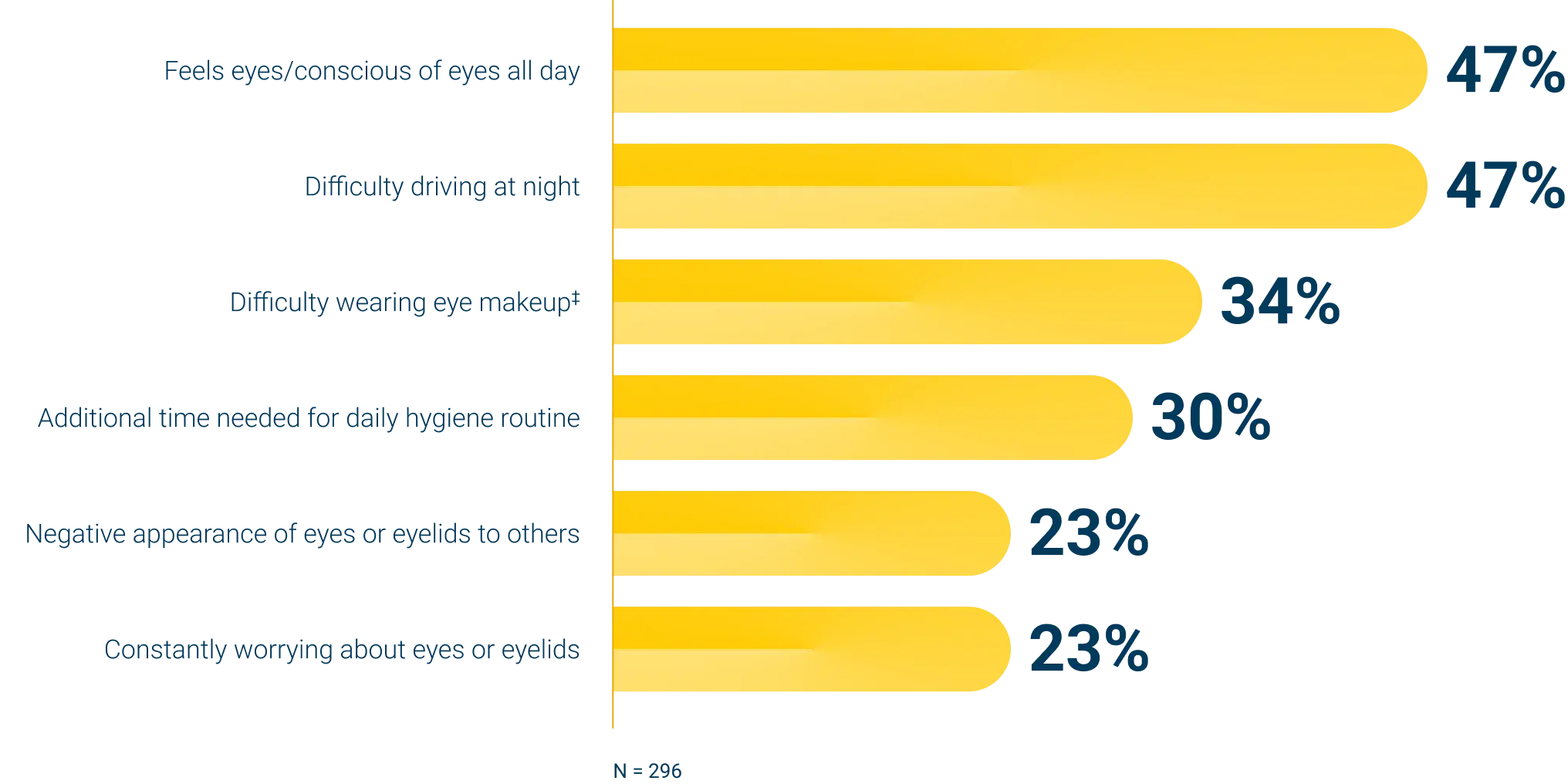
†Only impacts on daily life that were reported in greater than 10% of patients are listed here.
‡Women only.
DB can be confidently diagnosed by looking for collarettes during a routine slit lamp exam. When present, collarettes are easily seen along the lash line of the upper eyelid margin when your patient looks down.1
Slit lamp evaluation, 1.0x magnification
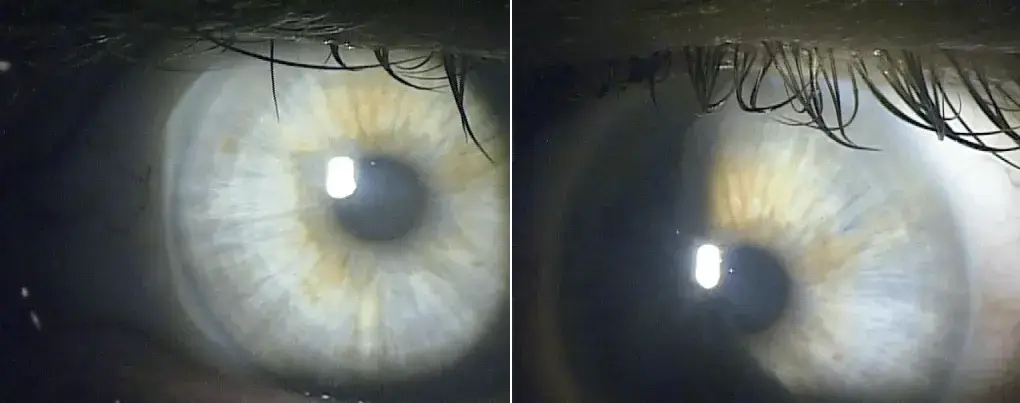
Patient looking straight ahead.
Patient looking straight ahead with lid lift.
Slit lamp evaluation, 1.0x magnification

Patient looking down, diffuse collarettes.
MGD is a chronic eyelid condition, often associated with Demodex infestation, that affects millions of Americans.11,12
Demodex mites are key contributors to MGD in patients with DB, causing inflammation and reduced meibomian gland function.11,13,14
Video Credit: Elizabeth Yeu, MD
1. Trattler W, Karpecki P, Rapoport Y, et al. The prevalence of Demodex blepharitis in US eye care clinic patients as determined by collarettes: a pathognomonic sign. Clin Ophthalmol. 2022;16:1153-1164. 2. Fromstein SR, Harthan JS, Patel J, Opitz DL. Demodex blepharitis: clinical perspectives. Clin Optom (Auckl). 2018;10:57-63. 3. O’Dell L, Dierker DS, Devries DK, et al. Psychosocial impact of Demodex blepharitis. Clin Ophthalmol. 2022;16:2979-2987. 4. Symphony Health Claims Data. 5. Market Scope 2020 Dry Eye Products Report: A Global Market Analysis for 2019 to 2025. 6. White DE, Zhao Y, Ogundele A, et al. Real-world treatment patterns of cyclosporine ophthalmic emulsion and lifitegrast ophthalmic solution among patients with dry eye. Clin Ophthalmol. 2019;13:2285-2292. 7. Statement: American Academy of Ophthalmology and ASCRS Urge Aetna to Reverse Disruptive New Policy on Cataract Surgery. American Academy of Ophthalmology. Published July 1, 2021. Accessed September 30, 2024. https://www.aao.org/newsroom/news-releases/detail/aetna-urged-to-reverse-policy-on-cataract-surgery 8. Why contact lens wearers need their annual eye exam. Eye Health. Published May 29, 2017. Accessed September 30, 2024. https://americanrefractivesurgerycouncil.org/contact-lens-problems-it-might-be-contact-lens-intolerance 9. Li J, O’Reilly N, Sheha H, et al. Correlation between ocular Demodex infestation and serum immunoreactivity to Bacillus proteins in patients with facial rosacea. Ophthalmology. 2010;117(5):870-877. 10. Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089-3094. 11. Liu J, Sheha H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505-510. 12. Sun M, Moreno IY, Dang M, Coulson-Thomas VJ. Meibomian gland dysfunction: what have animal models taught us? Int J Mol Sci. 2020;21(22):8822. 13. Pitts J, Lievens C. Put the squeeze on meibomian gland disease. Review of Optometry. Published September 16, 2009. Accessed September 30, 2024. https://www.reviewofoptometry.com/article/put-the-squeeze-on-meibomian-gland-disease 14. Zhang XB, Ding YH, He W. The association between Demodex infestation and ocular surface manifestations in meibomian gland dysfunction. Int J Ophthalmol. 2018;11(4):589-592.
Our Terms of Use and Privacy Policy have changed.
By clicking accept, you agree that you have read and will abide by these new terms.